Barrett's Esophagus Specialists: Expertise That Matters
Barrett’s Esophagus is manageable with early detection and proper care.
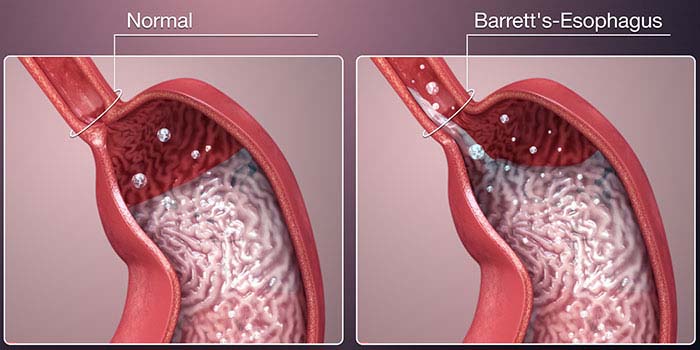
Barrett’s Esophagus is a serious condition in which the normal tissue lining the esophagus changes to resemble the lining of the intestine. This transformation, often a result of chronic gastroesophageal reflux disease (GERD), increases the risk of developing esophageal adenocarcinoma, a rare but aggressive form of cancer. Because of its complexity and potential risks, seeking care from a Barrett’s Esophagus specialist is essential for accurate diagnosis, ongoing monitoring, and effective treatment.
Understanding Barrett’s Esophagus
Barrett’s Esophagus often develops silently. Many patients may not even realize they have it until it is discovered during an endoscopy for persistent GERD symptoms. The primary concern with Barrett’s is its potential to progress from metaplasia (a change in cell type) to dysplasia (abnormal cell growth) and eventually to cancer. Fortunately, with proper surveillance and intervention, this progression can often be prevented.
Why See a Barrett’s Esophagus Specialist?
General gastroenterologists can manage many digestive disorders effectively, but Barrett’s Esophagus requires a higher level of expertise due to its cancer risk and evolving treatment options. A Barrett’s specialist is typically a gastroenterologist with additional training and experience in:
-
Advanced Endoscopic Imaging: Specialists use high-definition endoscopy, narrow-band imaging (NBI), and confocal laser endomicroscopy to detect subtle changes in the esophageal lining.
-
Targeted Biopsies: Regular biopsies are critical for monitoring dysplasia. Specialists know how to obtain and interpret these accurately.
-
Radiofrequency Ablation (RFA) and Endoscopic Resection: These are minimally invasive procedures used to treat dysplasia and remove early cancerous lesions.
-
Multidisciplinary Management: Specialists coordinate with pathologists, oncologists, and surgeons to provide a comprehensive care plan, especially if cancer is detected.
Key Diagnostic Tools and Treatments
A Barrett’s Esophagus specialist employs a variety of tools to diagnose and manage the condition. Some of the most commonly used techniques include:
-
Upper Endoscopy (EGD): The gold standard for diagnosing Barrett’s. It allows the doctor to visually inspect the esophagus and take biopsies.
-
Esophageal pH Monitoring: Assesses acid reflux, a major contributor to Barrett’s development.
-
Endoscopic Ultrasound (EUS): Helps determine the depth of abnormal tissue and whether lymph nodes are involved.
-
Endoscopic Mucosal Resection (EMR): Used to remove early-stage cancer or high-grade dysplasia.
-
Radiofrequency Ablation (RFA): Destroys abnormal tissue with controlled heat while preserving healthy tissue underneath.
Personalized Surveillance Strategies
Barrett’s Esophagus does not follow a one-size-fits-all approach. A specialist will assess the extent of Barrett’s, the presence of dysplasia, and individual patient risk factors to determine a surveillance schedule. Typically, patients with non-dysplastic Barrett’s are monitored every 3–5 years, while those with low-grade or high-grade dysplasia may need more frequent endoscopies or treatment.
Surveillance and treatment guidelines are updated regularly as new evidence emerges, making the expertise of a Barrett’s specialist critical for up-to-date care.
Finding a Barrett’s Esophagus Specialist
Barrett’s Esophagus specialists often work at academic medical centers, cancer institutes, or specialized gastrointestinal clinics. Leading institutions such as the Mayo Clinic, Cleveland Clinic, and Johns Hopkins have dedicated Barrett’s and esophageal cancer programs. These centers offer not only expert physicians but also access to clinical trials and emerging treatments.
When choosing a specialist, consider:
-
Board Certification and Training: Look for gastroenterologists with additional training in advanced endoscopy or esophageal disease.
-
Experience with Barrett’s: Ask how many patients they treat annually and what technologies they use.
-
Collaborative Care: Ensure they work with a multidisciplinary team if cancer care becomes necessary.
-
Patient Communication: A good specialist explains complex procedures and options clearly, empowering patients to make informed decisions.
Looking Ahead
Barrett’s Esophagus is manageable with early detection and proper care. Specialists play a pivotal role in preventing the progression to cancer through vigilant monitoring and timely interventions. With ongoing advances in endoscopic technology and a better understanding of risk factors, the outlook for patients with Barrett’s has improved significantly.
If you have chronic GERD or a family history of esophageal cancer, it may be time to talk to a Barrett’s Esophagus specialist. Their focused expertise could make a life-saving difference.